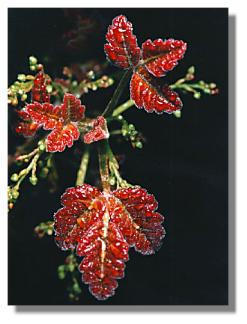
Psoriasis is a chronic noninfectious skin inflammation involving keratin synthesis that results in psoriatic patches, characterized by the eruption of circumscribed, discrete and confluent, reddish, silvery-scaled maculopapules. The lesions occur predominantly on the elbows, knees, scalp, and trunk.
Psoriasis most commonly begins between ages 15 and 35 and it can appear suddenly or slowly.
Type of Psoriasis
There are five main types of psoriasis.
- Erythrodermic: The skin is redness and covers a large area.
- Guttate: The skin appears small, pink-red spots.
- Inverse: Skin redness and irritation occurs in the armpits, groin, and in between overlapping skin.
- Plaque: Thick, red patches of skin are covered by flaky, silver-white scales. This is the most common type of psoriasis.
- Pustular: White blisters are surrounded by red, irritated skin.
Symptoms:
- Pruritus
- Shedding, silvery, white scales on a raised, reddened, round plaque that mostly affects the scalp, knees, elbows, extensor surface of arms and legs, and sacral regions.
- A yellow discoloration, pitting, and a thickening of nails if they are affected.
- Joint inflammation with psoriatic arthritis.
Nursing Intervention:
- Administer daily soaks and tepid, wet compresses to the affected areas to remove scales.
- Assist the client to remove the scales during the soak.
- Occlusive dressing may be applied following application of corticosteroid to increase its effectiveness
- Plastic wrap or bags can be used as occlusive dressing.
- Instruct the client not to scratch the affected areas and to keep the skin lubricated to minimize itching
- Encourage client to wear light cotton clothing over affected areas.
- Instruct the client to be consistent regarding prescribed treatment and avoid over the counter medications.
Treatment for psoriasis can be intralesional therapy (injection of triamcinolone acetonide, aristocort, kenlog-10, trymex), systemic therapy (methotrexate, hydroxyurea, and cyclosporine A), and photochemotherapy.
Read more...